|
REPORTS
|
|
“INNOVATION AND DEVELOPMENT IN HEALTH: INTEGRATION
OF COMPLEMENTARY AND TRADITIONAL MEDICINE
IN PUBLIC HEALTH SYSTEMS” 28-31 OCTOBER, FLORENCE, ITALY |
Roberta Pellizzoli [*] and Giulia Dario [°] In 1978, the World Health Organization (WHO), in the Declaration of
Alma Ata on primary health care, appealed to the international community
to support the inclusion of complementary medicine and traditional therapies
of scientifically-proven effectiveness in national health systems, on
the basis that they can reduce the consumption of conventional pharmaceuticals
and thus costs of public health systems. Moreover, not only can traditional
medicines reduce patients’ adverse responses to conventional drugs,
but their production and use is a way to contribute to the development
of local economies and to the sustainability of health services. Thirty
years later, on the anniversary of the Declaration of Alma Ata, this International
Workshop has been the occasion to share and discuss experiences of integrating
complementary and traditional medicine (CTM) and to reassert the importance
of these practices. At international level, ART IDEASS is promoting methodologies aimed at
including traditional medicine in national health systems. Several technology-transfer
actions have been implemented with the support of the health services
of the Tuscany Region. In particular, ART IDEASS is promoting the methodologies
adopted by the National Department of Natural and Traditional Medicine
of the Cuban Ministry of Health, which has generated great international
interest. Building on this ongoing collaboration, the workshop’s
strategic aim was to inform representatives of Ministries of Health of
these innovative primary health practices, stimulate a broad exchange
of experiences and generate new demands for adopting this approach. The first session focused on analysing the response that complementary and traditional medicine has generated in public health systems. Precious Matsoso, from the WHO Secretariat on Public Health, Innovation and Intellectual Property, stressed the need for a common language between conventional and traditional medicine that could facilitate understanding and the need to develop appropriate methods and approaches of research, so that the safety and efficacy of herbal products can be controlled. After a seminal lecture from Edgar Morin (see the section “Critical concepts” of this issue for the full script), Nila Heredia of the Executive Secretariat for the Andean Health Organism called for a change in the dominant paradigm of conventional medicine towards a more holistic approach that defines health not just as lack of illness, but rather as wellbeing in the biological, spiritual and social sphere of every human being. A key concept, in her presentation, was that of interculturality, understood as the process of creating “another” knowledge, “another” political practice, “another” society, to create a balance between all human beings and the environment in which they live and to achieve health for all. In this respect, interculturality is not only a tool for reducing costs and commercializing traditional medicines but is important for the articulation of different - conventional and traditional - forms of knowledge and practices that should not be hierarchically organized. The second session dealt with the main aspects of a national strategy for the inclusion of CTM in public health systems and Elio Rossi, for the Tuscany Network of Complementary Medicine, discussed the concrete steps and the role of key actors needed for putting in place such a strategy. Marta Pérez Viñas, director of the Centre for the Traditional Medicine of the Health Ministry in Cuba, provided a concrete example of how this strategy can be designed and implemented, presenting the articulated experience of Cuba, where a plan to use CTM for helping victims of natural disasters has been recently developed. Other experiences of integration of CTM in the public health systems were presented in the third and fourth sessions, where speakers from Sri Lanka, South Africa, Afghanistan, Mali, Ecuador, Bolivia, Venezuela, Chile, Guatemala, Dominican Republic, Serbia, Mozambique, Albania, Iran and Morocco discussed projects, problems and prospects in their own countries. The fifth session highlighted “Specific topics related to the implementation of a national strategy for the inclusion of CTM in public health systems”. Rita Cassisi, from UNIFEM Mexico, stressed the relevance of the production of medical plants not only for local economic development but also to empower women: women, she underlined, have an in-depth knowledge of the environment in which they live, including a specific knowledge of the indigenous plants and of their use in medicine that should be recognized and enhanced. Lourdes Acosta, from the Centre for Traditional and Natural Medicine of the Health Ministry of Cuba, focused on her country's experience of training human resources to use natural medicine in addressing epidemic diseases. According to her, a key factor for a successful strategy of integrating CTM is having university- level training in using traditional medicine and techniques. In Cuban universities, in fact, students can choose to qualify in Natural and Traditional Medicine. These skills have been successfully used to address epidemic diseases such as hemorrhagic dengue fever or hepatitis A with homeopathy, acupuncture or flower therapy. Another major challenge relates to the need of exchanging experiences and practices in South-South cooperation networks, together with an increased role of research institutes and Universities as Dr. Precious Matsoso (WHO) stressed in an interview:
Interview with Precious Matsoso, Director, WHO Secretariat on Public Health, Innovation and Intellectual Property: The important role of universities in disseminating knowledge on CTM
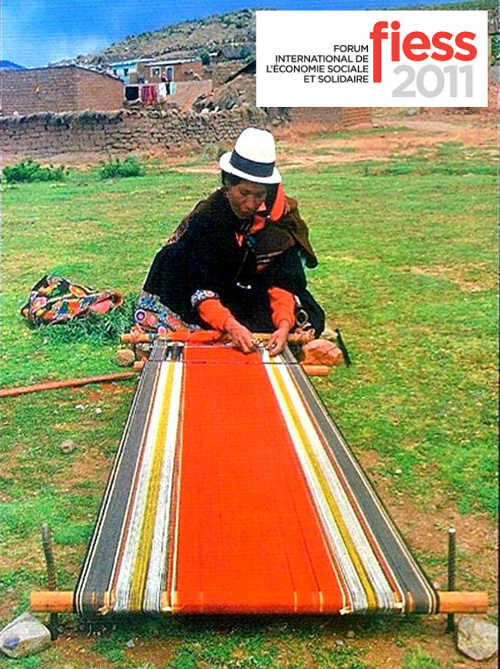
was also emphasized by Nila Heredia who, referring to case of Bolivia,
highlighted how the election of an indigenous President, Evo Morales,
has been the starting point for a new and progressive approach towards
the strengthening of intercultural practices. The Bolivian section of
the Andean Health Organism, in fact, is leading several projects aimed
at including intercultural education in the Faculties of Medicine and
at organizing courses for the non-graduated staff working in the health
sector. While recognizing that there are some aspects in the Bolivian
intercultural experiences that need to be improved, Heredia argued that
exchanging strategies and practices is crucial for the improvement of
the health sector. The experiences of Bolivia and of other countries demonstrated
how important it is to find spaces for the exchange of accumulated knowledge
and to expand networks and partnerships at all levels. The last session
was intended as a space for open discussion and for advancing proposals
to build concrete cooperation prospects for the inclusion of CTM in public
health systems. The draft of the final declaration was discussed, and
countries interested in receiving cooperation on CTM issues presented
their requests. The Final Declaration stresses that health systems must
be adapted and responsive to an intercultural approach to health and disease:
within this approach, complementary and traditional medicine is an important
tool for empowering and enriching the capacity of public health systems
and improving quality of life. It was underlined that CTM can make health
systems more comprehensive and preserve cultural diversity, thus contributing
to human development. Importantly, this Declaration gave birth to the
“International network for the integration of complementary and
traditional medicines in public health systems” and proposed the
establishment of a Cooperation Programme to support its activities[2]
. |
* Roberta Pellizzoli, PhD candidate in “International Cooperation and Sustainable Development Policies”, University of Bologna, is Editorial Administrator of Universitas Forum. ° Giulia Dario is Coordinator of the ART/Ideass Programme (UNDP/UNOPS). 2. For the full text of the declaration see: http://www.ideassonline.org/pic/doc/DeclarationENG.pdf |
Universitas Forum, Vol. 1, No. 1, December 2008
|
Universitas Forum is produced by the Universitas Programme of the KIP International School (Knowledge, Innovations, Policies and Territorial Practices for the UN Millennium Platform).
Site Manager: Archimede Informatica - SocietГ Cooperativa
В